
Building unity through service — Helping mankind is at the heart of the teachings of the Bahá’í faith. Find out what a Reston-based community is doing to serve humanity in big and small ways. [Reston Association]
An early warning for Metro riders — Although this year’s Cherry Blossom Festival won’t directly impact the Silver Line, August may be a rough ride. Service will be significantly reduced beginning August 11. [WMATA]
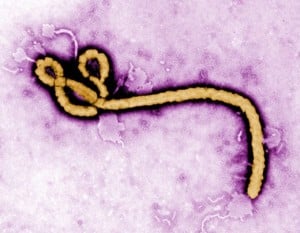
Ebola, a monkey house and a throwback to 1989 — Here’s a blast from the past: a story about when the most dangerous strand of ebola, a silent killer, lurked in Isaac Newton Square. [WETA]
Photo by Angelika Stadel
Gloria Addo-Ayensu, Director of Health for the Fairfax County Health Department says that the county, particularly in the wake of a scare at Inova Fairfax Hospital earlier this month, is keeping apprised daily with recommendations on controlling the deadly disease.
A woman who vomited on a tour bus near the Pentagon Oct. 17 was sent to Inova Fairfax after Virginia Hospital Center in Arlington refused to treat her. It was later determined the woman did not have Ebola.
Below is the statement from Add0-Ayensu, issued Monday:
Dear Fairfax Area Community,
The constant media coverage of the Ebola cases that were diagnosed in Texas and New York continue to fuel concerns among people in the general population and have highlighted risks in health care settings.
Adding to these concerns is the Ebola scare that occurred in the Fairfax area on Friday, October 17, which involved a suspect Ebola patient who was transported from the Pentagon to Inova Fairfax Hospital. Although it was a false alarm, I’d like use the incident to help increase public understanding about how the public health system works and also provide an update about our Ebola readiness.
One of the critical early decisions that must be made when evaluating a suspect case of any disease is whether the individual meets the case definition and therefore warrants confirmatory testing. For Ebola virus disease (EVD), the decision to test is based on the patient’s travel history, determination of exposure risk, and whether the symptoms are consistent with EVD.
The process for testing at the Centers for Disease Control and Prevention (CDC), if necessary, is facilitated by local health departments. While it took some time to validate travel history of the individual involved in the October 17 incident, fortunately, doctors at Inova gathered enough information to determine that the patient did not have any exposures to Ebola and therefore testing was not required.
 (Update, 6 p.m. Tuesday). Virginia Hospital Center has issued a statement about the incident. Read it on ARLnow.com.
(Update, 6 p.m. Tuesday). Virginia Hospital Center has issued a statement about the incident. Read it on ARLnow.com.
The woman suspected of having Ebola and taken to Inova Fairfax Hospital on Friday was taken there from the Pentagon because the nearest facility, Virginia Hospital Center in Arlington, refused to treat her, ARLnow.com reports.
The Arlington County Fire Department told ARLnow.com that VHC refused the woman — who at the time was thought to potentially have the deadly Ebola virus — when medics brought her to the hospital. She never left the ambulance.
“We were turned away,” said ACFD spokeswoman Lt. Sarah Marchegiani. “We followed our protocol and brought the patient to the closest hospital (VHC), at which point we were rerouted to Fairfax Inova.”
The woman, who was not identified, vomited on a tour bus near the Pentagon Friday morning and set off quarantines across the region. Medical officials said late Friday the woman did not have Ebola. They also said she had not traveled to West Africa, as she first told authorities.
“Based on the public health investigation, which included the travel history of a woman who became ill this morning in a Pentagon parking lot, and on questioning of her by medical staff, medical authorities are confident that she does not have Ebola,” officials said in a statement.
However, the situation brings up questions on whether hospitals in the area — and across the United States — are prepared to handle Ebola. Earlier this month, VHC said it was prepared for Ebola patients.
Said the hospital in a statement:
“Virginia Hospital Center wants to reassure our community that the Hospital has the infrastructure and procedures already in place to screen, and if necessary, isolate, test and treat all high-risk patients. We drill and prepare for just such situations; therefore, our staff is highly trained to take appropriate precautions for a suspected and/or confirmed Ebola case.
A multi-disciplinary task force has reviewed our infection control guidelines and reinforced education of the Hospital staff to ensure it can detect a patient with Ebola Virus Disease, protect all healthcare workers so they can safely care for the patient, and respond to the patient in a timely manner.”
Witnesses told ARLnow.com there was a “heated exchange” between the emergency physician and hospital administration inside the emergency room while the patient waited in the ambulance. The tipster also claims hospital administration worried it would lose business if it came to be seen as an “Ebola hospital.”
Meanwhile, the Centers for Disease Control on Monday issued new guidelines for health care facilities after it was determined staffers at Texas Health Presbyterian in Dallas were not given proper guidance when treating Thomas Eric Duncan, a man who had recently traveled to Liberia, when he presented with Ebola symptoms. Duncan has since died, and two nurses who treated him are also being treated for the disease.
Reston Hospital Center and Inova Fairfax said last week they are taking extra precautions should an Ebola case need treatment here.
ARLnow.com reporters contributed to this article.
 As fear over Ebola spreading in the United States has increased during the last several weeks, researchers Jerry and Nancy Jaax were reminded of another time and place: Reston in October of 1989.
As fear over Ebola spreading in the United States has increased during the last several weeks, researchers Jerry and Nancy Jaax were reminded of another time and place: Reston in October of 1989.
Twenty-five years ago, the husband-and-wife researchers, then working for the United States Medical Research Institute of Infectious Diseases (USAMRIID), were called to Reston, where monkeys in a lab at Isaac Newton Square’s Hazleton Labs had contracted a puzzling deadly disease.
That disease is now called Ebola Reston. The Jaaxs’ contributions were chronicled in the bestselling book, The Hot Zone.
The Jaaxes were part of the team that determined how Ebola Reston was spread (contact with an infected animal), why some humans tested positive but never got sick, how to keep it from spreading and how to effectively disinfect the lab where hundreds of monkeys either died or were euthanized.
Ebola Reston remains the only one of the five forms of the disease that is not fatal to humans. Ebola Zaire is the strain that has killed close to 2,500 persons in West Africa this year.
One man, Thomas Eric Duncan, contracted the disease in Liberia. He traveled back to the U.S. and, after initially being sent home, was treated at a Texas Health Presbyterian Hospital in Dallas. He died on Oct. 8. Meanwhile, two nurses who treated Duncan also contracted the disease.
Jerry Jaax, who is now Kansas State University’s associate vice president for research compliance as well as a university veterinarian, says that the Dallas hospital — and all U.S. hospitals — need to be prepared for all possibilities.
“There was no real excuse for a major hospital not to have some meetings and a team of people to handle this,” he said in a phone interview on Monday. “It was inevitable that someone would walk off a plane and present at a U.S. emergency room. I would think they would at least have had a skeleton plan and basic equipment.”
Here is what else the Jaaxes had to say about Ebola Reston, Ebola in the U.S. and the future of the disease.
Q: Have things changed much in infectious disease since the late 1980s, when Ebola Reston was discovered?
Jerry Jaax: Yes and no. When the outbreak was discovered in Reston, there were only two kinds of Ebola. Zaire (the type that is affecting Africa now) and Sudan, which has a very high mortality rate. When we were called to Reston, Ebola had never been reported in monkeys.
When you look at all the angst in this county now, back then only 1 out of 1,000 people had ever even head of Ebola. There wasn’t this tremendous response. There wasn’t the media coverage, which has really ratcheted up the fear.
In retrospect, it made what we were doing a lot easier. We were able to do our thing in relative anonymity. We absolutely were not ready for anything to happen. We really had to cobble together a response in a short period of time. We had to go down [to Reston] and not get people sick.
Read More
Update at 5:20 p.m. — The woman who vomited on a tour bus near the Pentagon Friday morning and set off quarantines across the region does not have Ebola, Fairfax and Arlington health department officials said Friday evening.
“Based on the public health investigation, which included the travel history of a woman who became ill this morning in a Pentagon parking lot, and on questioning of her by medical staff, medical authorities are confident that she does not have Ebola,” officials said in a statement.
(Updated at 5:00) A woman vomiting on a tour bus near the Pentagon Friday morning is being evaluated for possible symptoms of Ebola at Fairfax Inova Hospital.
County health officials said the woman is being kept in isolation while they get information about her health and travel history. Local health departments are working to find every person who had contact with the woman.
“The patient was immediately isolated and is undergoing triage in consultation with the Fairfax County Health Department,” Inova said in a statement. “Based upon that evaluation, a decision will be made by the health department as to whether the patient meets the criteria to be tested for the Ebola virus.”
The Centers for Disease Control will determine whether the woman should be tested for Ebola, Fairfax County Health Department officials said about 3 p.m.
The woman, whose age was not released, became ill on a tour bus in the Pentagon’s south parking lot about 9:10 a.m. Friday, according to a statement from Arlington County. When medics learned she had recently arrived from Africa, a hazardous materials team was called out of “a complete abundance of caution,” Pentagon Force Protection Agency spokesman Chris Layman told ARLnow.com.
The woman was initially taken to Virginia Hospital Center but did not exit the ambulance. The Arlington County Fire Department then transported her to Fairfax Inova Hospital, Arlington officials said. A news chopper photographer posted photos of emergency vehicles and an orange protective tent outside the 3300 Gallows Rd. hospital about 12:15 p.m.
PHOTOS possible #Ebola patient moved to #Fairfax hospital from the Pentagon #BREAKING #BreakingNews pic.twitter.com/AdFbiLafHK
— Brad Freitas (@NewsChopperBrad) October 17, 2014
We are aware of the possible #Ebola patient taken to Inova Fairfax Hospital. We are actively monitoring the situation.
— FairfaxCounty Health (@fairfaxhealth) October 17, 2014
The possible Ebola patient is currently in isolation while confirmation of her travel history and medical condition are being conducted.
— FairfaxCounty Health (@fairfaxhealth) October 17, 2014
Health Depts. around the region are now mobilizing to locate individuals who may have had contact with the patient. Updates TK.
— FairfaxCounty Health (@fairfaxhealth) October 17, 2014
UPDATE: @CDCgov has been contacted by @VDHgov to determine whether testing of this individual is warranted. http://t.co/2ju9Ee2lo9
— FairfaxCounty Health (@fairfaxhealth) October 17, 2014
Two officials with knowledge of the incident, plus the woman’s boss at a public relations firm, said they do not believe the patient had recently traveled outside the U.S., The Washington Post reported. Rather, the woman was suffering from a “severe illness” and might have boarded the wrong bus, her boss said.
The bus the woman briefly rode was quarantined for four hours near Barracks Row in D.C. and D.C. police closed an entire block, the Post reported. D.C. Department of Health officials told U.S. Marines and others on board — who had no contact with the woman — to take their temperatures twice a day for the next three weeks and report any irregularities.
An Inova representative said Thursday that he was “absolutely confident” the facility could treat Ebola patients. Officials said then that they planned to open a separate Ebola unit next week.
A Loudoun county inmate who had recently traveled in West Africa was taken to Inova Loudoun Hospital on Thursday after she was found to have a low-grade fever, the Post reported. The middle-aged woman “didn’t meet the threshold for Ebola testing,” the hospital said in a statement Friday morning. “All safety precautions and protocols were in place” at the Loudoun hospital, they said.
 As more rigorous screenings for Ebola began at Dulles International Airport on Thursday, local hospitals said they’re ready to handle patients.
As more rigorous screenings for Ebola began at Dulles International Airport on Thursday, local hospitals said they’re ready to handle patients.
Reston Hospital Center is giving health care workers gowns and goggles, as the Centers for Disease Control and Prevention recommends, officials told WTOP. Staff will use respirator masks while in contact with people who could have the virus, and will follow World Health Organization guidelines.
Inova Fairfax Hospital will open a separate Ebola unit next week that can isolate as many as 12 people, WTOP reported. Inova Health System Chief Medical Officer Loring Flint said he was “absolutely confident” the facility could treat Ebola patients.
No cases of Ebola have been found in the Washington, D.C. region. Thomas Eric Duncan, the first ebola patient diagnosed in the U.S., had a three-hour layover at Dulles on Sept. 20, before he fell ill.
“The risk of Ebola spreading widely in the United States is low,” county officials said in a statement released Wednesday. Officials reminded residents that the virus is transmitted only by touching blood or bodily fluids of an infected person, touching contaminated objects or touching infected animals.
Heather Robertson’s obstetrician couldn’t find a single pair of medical gloves in the capital of Liberia.
An international development professional and Reston resident, Robertson worked in Monrovia for more than three years and received prenatal care from Dr. Rick Sacra, the Massachusetts doctor who contracted ebola this summer and tested negative, his doctor said Sunday.
When Robertson heard that Sacra raced from shop to shop in search of gloves this summer, she felt hopeless — and then figured out how she could help.
Robertson, 39, is collecting thousands of gloves in Reston and sending them to hospitals in Liberia grappling with the deadly ebola virus. Just three weeks after launching a Facebook page called Gloves for Love Liberia, Robertson has received more than 42,000 gloves donated from as far away as Australia and France.
“It’s exceeded all my expectations,” she said, noting her family is using their guest room to store the stacks of cardboard boxes.
Boxes of gloves starting at $12 each and Tyvek suits that cost $13 each are part of an Amazon Wish List created by Robertson, who has worked on infrastructure and workforce development projects in Africa for 13 years.
“The Wish List is like a wedding registry,” she said, and allowed her to control the quality of the gloves according to what medical professionals in Monrovia told her they needed.
While what Liberia needs most to handle ebola is volunteer medical staff, Robertson said, glove donations let people without that expertise help, too.
“Donating gloves seemed more personal than giving money,” she said. “There’s something about the tangibleness of it.”
More than 14,000 of the gloves were sent earlier this month to an Episcopal church in Monrovia, which donated the supplies to nine clinics, Robertson said. And on Thursday, she and volunteers packed 22,000 of the gloves onto a truck headed toward a ship that will ferry the supplies to a Catholic church in Liberia’s capital. With the help of a nun Robertson knows, the gloves will go to 14 clinics. Church-run clinics often don’t receive government money, she said.
Robertson said she talks every day to Monrovia residents who survived the country’s 14-year civil war and are now grappling with the outbreak.
“People are scared,” she said. “They’re doing the minimum amount of interaction possible. Maybe they go to a store and the bank and then they go home. They’re going back into a protection and self-preservation mode.”
Reston made global headlines in 1990 when a strain of the virus was first identified at a lab in the locality and a monkey infected with it escaped.
Gloves for Love Liberia is now trying to collect a total of 50,000 through the end of this week.
“I’m going to keep going until people [in Liberia] tell me they no longer want to hear from me,” Robertson said.
 Even though the man with the first confirmed case of Ebola in the United States spent three hours at Dulles International Airport nearly two weeks ago, Fairfax County Health Department officials say local residents do not need to take action.
Even though the man with the first confirmed case of Ebola in the United States spent three hours at Dulles International Airport nearly two weeks ago, Fairfax County Health Department officials say local residents do not need to take action.
“Even though there has been a confirmed case of Ebola diagnosed in the United States, an outbreak of Ebola — like the one currently occurring in West Africa — is highly unlikely in the United States,” health department officials said in a statement.
The two main factors fueling the epidemic in West Africa are not present in the United States: a lack of infection control practices; and African burial rituals, such as washing the body of the deceased, the health department said.
The man, who flew from Liberia to Brussels, then Brussels to Dulles and then Dallas, was not ill during the flight so he was not contagious, the Centers for Disease Control said.
“The ill person did not exhibit symptoms of Ebola during the flights from West Africa and the CDC does not recommend that people on the same commercial airline flights undergo monitoring, as Ebola is contagious only if the person is experiencing active symptoms,” the Metropolitan Washington Airports Authority said in a statement on Wednesday.
Fairfax County Health adds:
To prevent the spread of infectious diseases, the United States has a public health system that on a daily basis rapidly identifies/isolates people suspected of being sick and finds/contacts people who have been potentially exposed to the sick person. Public health systems like this do not exist in the African countries currently affected by the Ebola outbreak.
Coming into contact with people who do not have symptoms of Ebola poses no risk, even if they have recently traveled to affected countries in Africa
There is no action that people who live in the Fairfax community need to take as a result of the Ebola case recently identified in Dallas, Texas or the Ebola outbreak in West Africa.
 The man who was diagnosed with Ebola at a Dallas-area hospital this week traveled through Dulles International Airport on his way back from Liberia, officials said.
The man who was diagnosed with Ebola at a Dallas-area hospital this week traveled through Dulles International Airport on his way back from Liberia, officials said.
The Metropolitan Washington Airports Authority said late Wednesday that the Centers for Disease Control has assured them that the man was not ill during his flight on Sept. 20 so there is no chance of transmission.
“The ill person did not exhibit symptoms of Ebola during the flights from West Africa and the CDC does not recommend that people on the same commercial airline flights undergo monitoring, as Ebola is contagious only if the person is experiencing active symptoms,” MWAA said in a statement.
United Airlines officials said they believe that the man traveled on the following flights: Brussels to Washington Dulles on Flight 951, and Washington Dulles to Dallas-Fort Worth on Flight 822.
The CDC said in a statement there is “zero risk of transmission on any flight on which the patient flew because he was not symptomatic until several days after his trip and could not have been contagious on the dates he traveled.”
The CDC added that while they feel it is unnecessary “for it or the airline to contact others who were on the patient’s flights, United is providing information about the flights United believes the patient took, based on information provided by the CDC. We are ensuring our employees have this information and suggest that any customers who have concerns contact the experts at the CDC for further information.”
A Texas television station says the man spent three hours on the ground at Dulles. The planes in which he traveled have since flown to 27 cities, reports ABC 13 Houston.
The man, identified by the Associated Press as Thomas Eric Duncan, remains hospitalized in Dallas. Family members, including children, he came in contact with since showing symptoms late last week, are under a 21-day quarantine.
Ebola has killed more than 2,900 people since the outbreak began in March, according to the CDC..
Meanwhile, Reston has been mentioned in many reports this week as a place where Ebola was previously found in the United States. That infection, which began in monkeys imported from the Philippines to a Reston lab in 1989, was transmitted through the air.
While hundreds of monkeys either contracted or were exposed to what is now called Ebola Reston, one of five strains of the deadly disease, Ebola Reston did not infect humans.
Read more about Ebola Reston in this Reston Now article.
 There is worldwide concern over the worst Ebola outbreak in history. The current outbreak has killed nearly 700 people in four African countries, according to the World Health Organization.
There is worldwide concern over the worst Ebola outbreak in history. The current outbreak has killed nearly 700 people in four African countries, according to the World Health Organization.
The hemorrhagic disease is half a world away, but when scientists study Ebola and how it spreads, they often look to Reston.
That’s right, Reston, Va. There is a strain of Ebola called “Ebola Reston,” because it was discovered here in 1990.
There are five types of Ebola that can kill humans. Ebola Reston was discovered to only kill moneys, though
However, that discovery came after a serious medical investigation, chronicled in the book The Hot Zone.
Here’s what happened:
In the fall of 1989, Hazelton Laboratories had a lab at 1946 Isaac Newton Square West, where KinderCare is now located. The lab did animal experiments.
There were already about 500 macaque monkeys housed at the facility when 100 more were flown from the Philippines, according to an article in the Internet Journal of Preventative Medicine.
A month later, 29 of the 100 quarantined monkeys had died. During a necropsy, a veterinarian found one monkey’s spleen had tripled in size and hardened and there was blood in the intestines. After conducting several other necropsies he diagnosed the deaths as being caused by simian hemorrhagic fever virus (SHFV), the Journal article said.
The Hazelton facility veterinarian then sent samples of the monkey tissues to the United States Medical Research Institute of Infectious Diseases (USAMRIID) for a conclusive diagnosis. Meanwhile, Hazelton lab workers began euthanizing the remaining animals, but sporadic deaths began occurring in several other rooms. Soon, 30 monkeys from a different shipment were dead.
More from the Journal: Read More

