Reston Hospital Center is spending nearly $20 million for upgrades and renovations as it prepares to enhance its robotic-assisted surgery program.
The project calls for constructing four new, larger operating rooms and modernizing other areas “to provide added capacity to Reston’s robust surgical offering which performs over 10,000 surgeries annually,” a news release said.
The design phase of the renovation, which will involve over 22,000 square feet of space, is scheduled to begin this summer.
“This infusion of capital will upgrade our surgical capability and capacity to help deliver a world-class surgical experience for our patients and surgical care teams,” John Deardorff, chief executive officer of the HCA Healthcare Northern Virginia market and Reston Hospital Center, said in the news release.
The Richmond-headquartered health care system said the changes will help serve more patients. The hospital expects surgeries to continue uninterrupted during the project, hospital spokesman Todd McGovern said in an email.
The new and upgraded operating suites will help improve patient outcomes through the adoption of emerging technologies and innovative surgical approaches to help reduce hospital stays and lessen recovery times. The added capacity will allow Reston Hospital’s care teams to treat more patients needing complex spine care, orthopedic care, and minimally invasive surgery across a range of surgical specialty areas such as bariatric (weight loss), colorectal, general, hepatobiliary, gynecologic, thoracic (lung), and urologic surgery.
The Food and Drug Administration and researchers previously shared concerns about various robotic surgeries, noting that although they’ve been taking place in the U.S. since 2000, patients should be aware of outcomes and available evidence.
Different types of surgical areas have been taking off. Based on one measure, the number of general surgery procedures conducted by U.S. hospitals rose from 10,000 in 2010 to 246,000 in 2017, according to a physicians’ estimate.
Some doctors also raised concerns about costs for rural hospitals, noting in December 2020 that despite advantages noted with the procedures, there’s still a lack of high-quality evidence in most areas.
The planned upgrades are in addition to the hospital projecting to spend $70 million on projects that include a new freestanding emergency department at 8240 Leesburg Pike in Tysons coming in 2022.

Two local service groups launched an outreach initiative on Tuesday (June 22) to help transport veterans to and from medical appointments.
The free service is being managed by the Reston-based Dulles Airport Transportation Association and its longtime partner NV Rides, a network of volunteer driver programs housed at the nonprofit Pozez Jewish Community Center of Northern Virginia.
With the initiative, the organizations hope to address one of the many issues that veterans face when seeking health care, exemplified by the cancellation of millions of medical appointments at Veterans Affairs medical facilities during the COVID-19 pandemic.
Although virtual visits have surged and vaccinations are rising, medical needs persist.
“The program hopes to harness the power of the special bonds that exist between the men and women who’ve selflessly served our country,” a press release announcing the launch says.
DATA and NV Rides were already collaborating to give veterans rides through their existing Veterans Connect program. This expansion is specifically dedicated to serving elderly veterans and those with disabilities.
Targeted toward veterans in Fairfax, Loudoun, and Prince William counties, the program is currently recruiting additional volunteer drivers, who can be veterans or other community members. Drivers utilize their own vehicles.
Interested individuals can visit the Veterans Connect Facebook page or contact Luke Frazza at [email protected] or 703-819-3459, and Karla Nativi at [email protected] or 571-455-2836 to volunteer or learn more.
“While veterans have long stepped up to support their brothers and sisters in arms, elderly veterans have told us they are more likely to take advantage of a volunteer ride provided by someone with whom they have literally or even figuratively shared a foxhole,” the press release said.
Before the pandemic, the NV Rides network provided about 1,100 rides per month to non-driving adults 55 and older, primarily in Fairfax and Loudoun counties, according to the group.
With stay-at-home orders last year, ridership declined by 60%, but partners continued to provide ride services to the most critical medical care appointments. Over the past year, ridership has bounced back, with the network providing over 1,500 rides last month, the organization says.
“We think this veteran-specific expansion of our NV Rides program will underscore our belief that our network provides ‘More than just a ride,'” NV Rides Manager Jennifer Kanarek said in a statement. “…Stories of joyful moments between volunteers and passengers are far more often the rule than the exception.”
Researchers have found that transportation can be a major barrier to accessing health care, a concern that has persisted in Fairfax County’s COVID-19 vaccine rollout.
The county is now offering a free weekend shuttle to and from its vaccine clinic on Route 1 in Alexandria. Other available transportation options include free taxi rides and rides for people 55 and older from the Shepherd’s Center.
In addition to the Veterans Connect program, DATA has also partnered with the nonprofit Northern Virginia Veterans Association to provide free rides to veterans for COVID-19 vaccine appointments, WDVM reported in May. That effort is being funded by an $80,000 grant from the Federal Transit Administration.
“The feedback we’ve received from local veteran service organizations has been nothing but positive,” Veterans Connect Mobility Manager Luke Frazza said in a statement. “Support for the project has transcended those who served however, and garnered praise from across our community.”

Reston Hospital Center has committed $70 million to a series of new initiatives that are expected to roll out over the next three years.
Building off of a multi-year expansion of the hospital’s campus near Reston Town Center that finished in early 2020, the projects aim to “expand service capacity, modernize facilities, and introduce state-of-the-art technologies to help meet the growing healthcare needs in the region,” the HCA Virginia Health System, which includes Reston Hospital, said today (Wednesday) in a press release.
The projects include a new, freestanding emergency room in Tysons that will serve as an extension of its existing services and a 13,000 square-foot expansion of the Inpatient Rehabilitation Center, which will go from 18 to 30 beds.
On top of the upcoming changes, Reston Hospital also started utilizing an augmented reality system to conduct spinal surgeries in October.
Here is a full breakdown of the new initiatives:
New Freestanding Emergency Department: Reston Hospital has commenced construction on a new standalone emergency room (ER), at 8240 Leesburg Pike. Located in the heart of Tysons, VA near the intersection of Route 7 and Route 123, this nearly 14,000 square-foot facility will be conveniently positioned within walking distance to both the Greensboro and Tysons Metro stations. The emergency department will be an extension of Reston Hospital Center and is targeted for a Q1 2022 opening. Upon launch, the 11-treatment room, state-of-the-art ER will be staffed with board-certified emergency room physicians and nurses, 24-hours a day, 365 days a year and offer the same services provided in an emergency room that is housed within the walls of a hospital.
Inpatient Rehabilitation Center Expansion: Reston’s Inpatient Rehabilitation Center will expand from 18 to 30 beds to support patients recovering from various debilities, including stroke, spine and brain tumors, traumatic brain injuries and other neurological conditions. This project will add 13,000 square feet to the all-private unit; construction will begin in late 2021, with an expected completion date in early 2023.
Facility Renovation and Modernization: Funds will be reinvested in the facility’s remaining patient care areas including women’s care services to refresh and modernize finishes; elevating the patient experience across the hospital. The project will also provide improvements to the hospital’s physical plant and infrastructure to improve system safety and reliability.
Surgical Technology Enhancements: Reston is continuing to enhance one of the region’s most advanced surgical service portfolios with significant investments in key areas including robotic surgery and augmented reality-guided surgery. These emerging technologies will enhance surgical patient experience through reduced hospital stays and shorter recovery times across many surgical specialties including bariatric (weight loss), colorectal, general, gynecologic, hepatobiliary (pancreas and liver), neuro, orthopedic, spine, thoracic (lung), and urological surgeries, among others.
Advanced Stroke Care: Reston has enriched their accredited primary stroke treatment program by opening its neurointerventional suite in the fall of 2020. The service is offered in partnership with the nationally-regarded neurovascular team from Medstar Medical Group.
Technology Upgrades: Additional funding has also been spent or earmarked for updates to cancer treatment technology for radiation therapy and diagnostic imaging system upgrades.
“These service expansions, investments and improvements are critical in helping us to continue delivering on our commitment as a premier specialty hospital, as well as being recognized as the healthcare provider and the employer of choice in the Northern Virginia region,” HCA Healthcare Northern Virginia and Reston Hospital President and CEO John Deardorff said.

Inova Health System will open a new cancer screening and prevention center on its Center for Personalized Health campus in Merrifield, thanks to a $20 million donation from Reston couple Paul and Linda Saville.
Paul Saville is the president and CEO of the Reston-based home construction company NVR, Inc.
Announced on Nov. 10, the new 24,000 square-foot cancer screening center will be an expansion of the Inova Schar Cancer Institute, which opened in May 2019 and bears the name of NVR founder and Chairman Dwight Schar and his wife Martha after they donated $50 million to build it, according to the Washington Business Journal.
“We’ve all been impacted by cancer, and many of us know someone who has died from cancer due to a late diagnosis,” Paul Saville said. “We hope that many more people will have access to early detection and treatment and avoid serious disease.”
Inova says the new center made possible by the Savilles’ donation will be the first of its kind in Northern Virginia, which currently lacks a “comprehensive, multidisciplinary, organized cancer screening and prevention program.”
Expected to open in fall 2021, the center will provide screenings to detect breast, lung, prostate, bladder, pancreatic, colorectal, head and neck, skin, cervical, uterine, ovarian, and other cancers.
Preventative resources for patients who may be at high risk of developing cancer will include genetic testing, opportunities for clinical trials, and education on nutrition and exercise.
“The Savilles’ commitment to help us create a state-of-the-art early detection and prevention center is bringing us a giant step closer to becoming the leading cancer institute in our region,” Inova Health System President and CEO J. Stephen Jones said.
The U.S. Centers for Disease Control and Prevention currently list cancer as the second most frequent cause of death in the U.S. after heart disease, but that appears to be based on data from 2018.
According to Inova, cancer surpassed cardiovascular disease as the leading cause of death in America this year.
“By providing members of our community accessible, multidisciplinary screening and prevention services in a ‘one-stop-shop’ approach, we hope to cure more cancers by catching them early,” Schar Cancer Institute President John Deeken said. “And through programs such as smoking cessation, as well as dietary and exercise interventions, we hope to prevent more and more cancers in the years ahead.”
Photo via Google Maps
Clinics and medical facilities are beginning to offer yearly vaccines as flu season approaches.
People who received their annual flu shot in a 2018 study were 82% less likely to be admitted to the ICU for potentially life-threatening symptoms, according to the Centers for Disease Control and Prevention’s website.
Most people six months and older can receive a dose of the flu shot, the Centers for Disease Control (CDC) said, adding that people can either choose the shot or the nasal spray.
The CDC suggests that those eligible should receive their yearly flu vaccine before the end of October.
Photo via Hyttalo Souza/ Unsplash
At the Reston Hospital Center, staff members are seeing a decline in both COVID-19 and non-COVID-related patients.
Compared to August of 2019, Reston Hospital Center Emergency Room admissions are down 20 percent and the hospital only had six COVID-19 patients currently, which is the lowest number since May, according to David Jacobs, the chairman and medical director for Reston Hospital Center’s emergency department.
But, this trend is concerning, Jacobs said — especially when it comes to non-COVID related visits.
The downward trend is partially due to people avoiding the emergency room in fear of catching COVID-19 at the facility. Additionally, people aren’t coming in close contact with others, and therefore avoiding catching other communicable diseases, Jacobs added.
Jacobs says he’s concerned over the drop in admissions since this means people might not be seeking help when they need it, leading to medical complications that otherwise would have been avoidable.
Examples of this include not being able to diagnose appendicitis in time or someone ignoring the beginning stages of a heart attack, Jacobs said.
To keep people safe when they come into the emergency room, the Reston Hospital Center has set up strict protocols, according to Jacobs. These include separating people with COVID-19 from other patients, use of personal protective equipment, regular temperature checks, the requirement of face masks for anyone who enters the building and frequent cleaning.
When considering a visit to the emergency room, Jacobs said there is little risk of catching COVID-19 at the facility since staff members stick to the health protocols set in place. It is far more dangerous to ignore symptoms and avoid seeking medical help, he said.
Jacobs said people should seek immediate medical attention when they notice warning signs such as:
- difficulty speaking
- unusual and sudden weakness in legs or arms
- chest pain
- new or worsening abdominal pain
One grievance Jacobs said he has heard repeatedly from patients is that they find it difficult to schedule a time to meet with their regular health care providers.
“I think the whole medical system is readjusting and struggling with how to safely see patients,” he said, adding that Reston Hospital Center has availability for people who need to be seen. “We are open and we have capacity.”
Practitioners are also concerned about an increase in drug and alcohol abuse.
“I think more people are out of work and have more time on their hands,” he said adding that people have also been coming in with mental health issues such as depression and suicidal thoughts that can feed off from stress associated with the pandemic.
Though the medical facility doesn’t have a detox center on-site, it does have medical professionals who can give consultations and direct people towards further help.
Some good news is on the horizon. Unlike elsewhere in the country, Jacobs said he hasn’t noticed a rise in child abuse or domestic violence cases at Reston Hospital Center.
“I’ve certainly heard and read about that but can’t say that I’ve experienced that or heard about a spike in the Reston area,” he said. “I think that’s an issue of concern that follows with a lot of these drug and alcohol and psychiatric related issues but I think to-date we haven’t seen a spike in our department.”
Going forward, Jacobs said he hopes people won’t avoid the emergency room because of fear over COVID-19, as hesitation could be deadly.
“We have five months of experience with this,” he said.
Photo courtesy Reston Hospital Center

Fairfax County’s Hispanic community is bearing the brunt of the COVID-19 pandemic.
Although Hispanic individuals comprise just under 17 percent of the total population, they account for nearly 66 percent of all confirmed cases in the county.
The rise has raised alarms about equity issues between different racial groups in the county. County health officials say that higher infection rates may be caused by the need to go to work, lack of sick leave, the inability to socially distance while on the job, and lack of unemployment insurance.
Cases have grown over the last three months in the Hispanic community, while efforts to flatten the curve in the black and white communities have been more successful, county data show.
“This risk reflects a group’s niche in society rather than a particular racial effect,” said Benjamin Schwartz, a medical epidemiologist with the Fairfax County Health Department.
Many local Hispanic residents work in jobs where the risk of transmission is especially high.
Roughly 25 percent of Hispanic men in the county work in natural resources, construction or maintenance, according to the 2018 American Community Survey. That’s compared to just five percent of blacks in the same industry.
Similarly, 45 percent of Hispanic women work in the service industry, more than double the percent of black women in the same industry, according to the survey.
Additionally, roughly 12 percent of Hispanic households are defined as overcrowded based on county metric, compared to four percent of the black community and less than one percent of the white community.
But the same racial disparity is not prevalent in other parts of the county. In Richmond, for example, blacks are being hit hard by the pandemic while poor whites are disproportionately impacted in southwestern Virginia.
On a national level, blacks account for a higher share of confirmed cases and deaths compared to the rest of the population, according to the Kaiser Family Foundation.
Roughly 20 percent of cases do not contain race and ethnicity information.
Exacerbating the Divide
At Cornerstones, a nonprofit organization based in Reston, the pandemic has exacerbated the daily struggle with housing, poverty, quality education, and living wage jobs.
Already, 33 percent of families in Cornerstones’ affordable rental housing have lost all or some of their income due to mass layoffs. Some have limited access to daycare and the internet, complicating long-distance learning, even if the school system provides a laptop for students.
Parking lots may offer free wifi access, but a car and time are needed to park there. Others turn to families and friends to watch their children, increasing the risk of exposure for all.
Public health officials are also seeking ways to improve community communication and increase testing in local hotspots, including the Town of Herndon.
In April, 385 new households came to Cornerstones’ pantry in need of food. That’s more than six times the number of new households in fiscal year 2019.
“For low-income members of the immigrant community in the time of COVID, it’s never one thing. The pandemic only exacerbates their daily struggling with housing, poverty, quality education, and living-wage jobs,” said Sara Newman, division director of community change partnerships at Cornerstones.
For these residents, the financial burden of COVID-19 is “inescapable,” Newman said.
“Unpaid rents are continuing to accumulate. People keep working or look for employment regardless of the viral spread so they can keep a roof over their family and food on the table.”
Photo by Morgan Von Gunten/Unplash
In times of uncertainty during the COVID-19 pandemic, many expectant mothers are facing unforeseen challenges.
Lack of knowledge around and educated guesswork around the coronavirus behalf of doctors can be unsettling — especially when dealing with the lives of newborn babies.
Around Reston, OBGYN offices such as the Virginia Women’s Health Associates in Reston are changing tactics to help new mothers and pregnant women stay safe by offering more online resources and flexible appointment dates for women who are experiencing flu-like symptoms.
The Virginia Women’s Health Associates are even offering online appointments through a new portal system.
For everyday care, local OBGYN offices are taking extra preventative measures to help patients respect social distancing measures and ensure the health of their patients.
Because of the lack of research doctors, such as Amy Banulis, a certified doctor out of Falls Church who published a professional article in the Northern Virginia Magazine, are recommending that expectant mothers be sure to practice self-isolation and be sure to take care of themselves not only physically but mentally as well.
“While there is currently no evidence that you are more likely than anyone else to be infected with COVID-19, you may be at higher risk of developing a severe case,” Banulis wrote. A similar statement can be found online from the Centers for Disease Control and Prevention (CDC).
When it comes to breastfeeding and other concerns, the CDC said breast milk usually provides protection against infection and has not been shown to transmit COVID-19 in “limited studies.”
A local mom in Falls Church said that she took extra precautions leading up to her delivery date.
“I just feel the research out there is limited. I’m skeptical and don’t want to take a risk,” Nicole Sud, who recently gave birth to twins at a Virginia Hospital Center, said.
Before her delivery date, Sud said she self-isolated — only leaving the house for doctor appointments and had neighborhood friends help deliver groceries and essentials. She said that her primary care doctor didn’t recommend any additional steps for keeping healthy beyond the CDC’s guidelines for the public.
When Sud was first checked into the hospital, said she doctors gave her one surgical mask and a paper bag to put it in. Surgical gloves that would typically sit by the sink in any doctor’s office had been removed because of thefts, Sud said.
After Sud delivered the twins, she was disappointed because the couple learned the hospital nursery was closed due to COVID-19 concerns.
To ensure that the couple’s two-year-old daughter didn’t catch anything at the hospital and pass it onto the newborns, her pediatrician suggested that the young girl live with Sud’s in-laws for two weeks before returning home.
Upon discharge from the hospital, nurses simply included a COVD-19 packet among other materials typically given to mothers, Sud said.
Photo courtesy Nicole Sud
Seventeen area high school seniors were recently awarded scholarships by the medical staff at Reston Hospital Center.
The student, who are from Fairfax and Loudoun County high schools, were recognized for academic excellence and excitement for pursue careers in healthcare.
RHC offers $15,000 in scholarships to local schools annually. The program has been in effect for the last 21 years.
“We are thrilled to be able to support these young adults as they venture into the world in search of their dream careers,” Dr. Avisesh Sahgal, president of Reston Hospital Center’s Medical Staff, said in a statement.
This year’s scholarship recipients are below:
- Ansel Sanchez – Briar Woods High School
- Lindsay Marie Burns – Broad Run High School
- Anna Kate Erstling – Chantilly High School
- Ashley Arely Reyes – Chantilly High School
- Lillian Tran – Dominion High School
- Riya Hadvani – Herndon High School
- Christopher Ngo-Khang Nguyen – James Madison High School
- Mariana Fernandes Gragnani – Langley High School
- Yanni George Conomos – McLean High School
- Maxmine Irmhild Ayompe-Mody – Oakton High School
- Jasmine Chiann Foo – Oakton High School
- Allison Armstrong – Park View High School
- Rayness Mollinedo-Rodriguez – Park View High School
- Chelsea Lazatin – Potomac Falls High School
- Nicole Post – South Lakes High School
- Olivia Nicole Chandler – Westfield High School
- Daisy Allison Lopez Rosa – Westfield High School
Photo via Reston Hospital Center
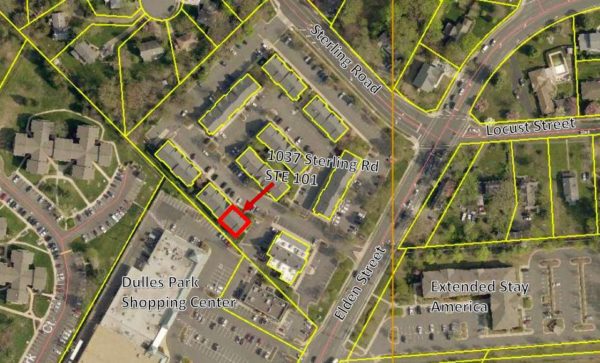
A vocational school for entry-level healthcare fields could be coming soon to the Crossroads (1037 Sterling Road, Suite 101).
The town’s planning and zoning staff recommended placing several restrictions on the proposal to open a Divine Healthtech Institute prior to approval. Vocational schools require a specific exemption from the town to operate in this area.
Conditions include holding no classes before 8 a.m. or after 10 p.m. and allowing town officials to inspect the property during “reasonable hours.”
“Staff maintains a level of concern with allowing multiple uses within one condominium suite from a general standpoint. In this specific case, staff believes the proposed use is similar enough to the existing use that any potential negative impacts could be mitigated by placing conditions on the approval,” according a the March 13 staff report.
If approved, the school would only be allowed to offer one class at a time in the 300-square-foot location. The condominium suite where the school would be located has a hodgepodge of uses, including two offices that are used for Nathan Travel and Cargo, a travel agency.
Rev. Leonard Chukwujiioke, a school administrator, said each class will have only five students. Weekend programs will be by appointment only. A morning and evening class will be offered on weekdays.
Most recently, the Herndon Town Council denied a plan to bring a mini-mart to the Crossroads last year. Plans for a barber shop were withdrawn after the town conditioned approval of the application with several requirements. The operation of a personal service business was approved last year.
The town’s Planning Commission will consider the plan at a 7 p.m. public hearing today (May 13).
Photo via handout/Town of Herndon
Reston Hospital Center is just under the halfway point of its $72 million expansion — on track and on budget for completion by the end of next year.
The completed pieces of the project include renovations of the Women and Children’s Services unit and expansion of the neonatal intensive care unit, along with new paint, flooring and upgraded equipment, Erin Echelmeyer, a hospital spokeswoman, told Reston Now. The West Wing Lobby is also finished, with a revamped lobby area, gift shop, physicians’ lounge and office space, she said.
“It is progressing right along,” Echelmeyer said. “We are on target to complete this second phase of our master facility plan by the end of 2019.”
A breakdown of the pieces of the project still in progress is below:
- New 18-bed Inpatient Rehabilitation Center
- Expanded 24-bed Intensive Care Unit
- Addition of a second lab to the cardiac services unit
- Renovations to visitor areas including a new cafeteria, a glass concourse, and main entrance and lobby
- New parking garage for patients and visitors on the West Wing entrance
- Addition of eight rooms to accommodate high-risk obstetric patients
Construction on a new 403-space parking garage has already begun, which is expected to be done by the end of next summer. The Inpatient Rehabilitation Center is slated to open next month, followed by the Intensive Care Unit in January, Echelmeyer said.
The hospital reopened the emergency room entrance, after having patients enter through the hospital’s main entrance, she said, adding that the emergency room, level II trauma center and pediatric emergency room “are all fully function[al] and accessible from the emergency room entrance.”
This is not the first time the 187-bed hospital, which is part of Tennessee-based health giant HCA Holdings, Inc, has expanded. The hospital embarked on a $40 million expansion between 2012 and 2015, which included a 180,00-square-foot medical office and the addition of four operating rooms and 19 surgical recovery rooms in the surgical department.
The current expansion was announced in 2016, when the hospital hit its 30th anniversary. The phased project will add more than 63,000 square feet of new space to the facility.
Photos Courtesy of HCA Healthcare

The medical staff of Reston Hospital Center awarded seventeen area high school graduates with scholarships this year. The awards are given to students to recognize their academic excellence and desire to pursue a career in healthcare.
RHC offers $15,000 in scholarships annually. At an award ceremony hosted by RHC, John Deardorff, President and CEO of RHC and HCA’s Northern Virginia Market, said, “These students are well deserving of the medical staff scholarships as they begin their journeys of exploring careers in the healthcare field. We hope that one day they return to their roots as members of our local medical community.”
The scholarship winners for 2018 are as follows:
- Natalie Rothrock – Briar Woods High School
- Jakob Cohen – Broad Run High School
- Ria Grover – Centreville High School
- Amara Novotny – Chantilly High School
- Arman Daneshpayeh – Chantilly High School
- Agota Banks – Dominion High Schoo
- Pranavi Palliniti – Dominion High School
- Yousef Hassan Elgodamy – Herndon High School
- Minnie Suki Nguyen – Herndon High School
- Katherine Elizabeth Priester – James Madison High School
- Yusuf Masser Bade – Langley High School
- Shreya Dalal – Oakton High School
- Khanh Nguyen – Park View High School
- Ashlin Rain Murphy – Potomac Falls High School
- Tashfia Anaan Emdad – Potomac Falls High School
- Aishwarya Jadhav – South Lakes High School
- Ruma S. Jadhav – South Lakes High School
Photo via RHC
 T
T
The Town of Herndon is aiming to become Virginia’s first dementia-friendly community in order to spread awareness about the impact of the disease on individuals.
Using a toolkit to engage community members, town officials and community partners aim to develop respect and inclusion of people with dementia. A dementia-friendly community also has services and resources throughout all community areas that promote quality life, educates people with dementia and their families and promotes engagement with the community.
There are 38 other communities in the Dementia Friendly America network, an initiative that includes more than 30 organizations to foster dementia friendly communities across the country.
Toni Reinhart, the owner of Comfort Keepers, a Herndon-based home health care service, is leading a team of community leaders throughout each phase of the initiative.
“With her to drive to enhance community awareness for persons with dementia and 16-year commitment to serving the Herndon-Reston area, her passion for senior care would only serve greater purposes statewide,” said Herndon Mayor Lisa C. Merkel.
Photo via DFAHerndon.org

Neuro-witchcraft — “A judge on Thursday appointed two brain experts to evaluate a man facing the death penalty in the slaying of a teenage Muslim girl last year, despite the objections of a prosecutor who derided the requests as “neuro-witchcraft.” Circuit Court Judge Randy Bellows agreed to the appointments of a neuropsychologist and neurotoxicologist to evaluate Darwin Martinez-Torres, 23, of Sterling, who faces charges including capital murder and rape in the June killing of Nabra Hassanen of Reston.” [WTOP]
More Metro inspections — New federal inspections find old Metro problems still persist, including several “code black” track conditions. [The Washington Post]
Stateside: On the front lines — Nurses are on the front lines in battling the opioid epidemic. One nurse says most of her patients are homeless. [The Connection]
Photo by Ressa Blair
The average age of a Reston adult is about 40, which means their parents are approaching retirement age.
While 40-somethings are focused on career and making sure their kids are getting prepared for college, are they also making sure their parents are prepared for retirement?
Our parents will inevitably need some form of long term care during their retirement years, so careful estate planning is important. Notably, the key word in estate planning is planning. Surprisingly, too many people do not have an adequate plan.
 I have found in my practice that many people mistakenly think Medicare covers all long term care expenses.
I have found in my practice that many people mistakenly think Medicare covers all long term care expenses.
However, Medicare (Part A) only pays for care in a long term care hospital, Medicare-certified skilled nursing facility under certain conditions for a limited time or through Medicare-certified home health services like intermitted skilled nursing care or hospice care. It will never pay for in-home custodial care, nursing home, continuing care retirement community, or assisted living facility.
Suppose your parent has dementia or Alzheimer’s and is fully mobile but cannot be left alone? Long term care for your parent can range from $2,000 to more than $6,000 a month. These costs are paid out of retirement funds and can easily exceed the average person’s retirement budget.
Although rare, there are organizations that provide affordable options like flat monthly fees for basic, mid-level and advance wellness packages to fit different budgets.
In some families, a family member becomes the caregiver, usually a spouse or a child. Even when family members step up to become the caregivers, respite or additional help is also frequently required. For those who plan ahead, purchasing long term care insurance is a great way to manage these costs while being able to remain in one’s home. Another option is designating a family member to be the care giver.
Consider what happens when your parent cannot afford the cost of care or does not have a family member to provide care. The only option is nursing home or home health care covered by Medicaid.
To qualify, your parent’s monthly income cannot exceed 300% of the SSI amount for an individual, or $2,205 per month for 2017 and Medicare will require any assets to be used to pay for care, unless the assets were transferred or liquidated 5 years prior to applying for Medicaid.
A popular strategy to deal with the 5-year “look back period” is to transfer the deed to the home to a child. This may solve the Medicare problem, but it has drawbacks. In most cases, the child will pay higher taxes if he or she later sells the property.
Be proactive in 2018. Contact us via email or call me at (703) 712-8000 set up a consultation and take the necessary steps to protect yourself and your family.